This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Borderline Personality Disorder: 4 Natural Ways to Help BPD Treatment
April 29, 2018

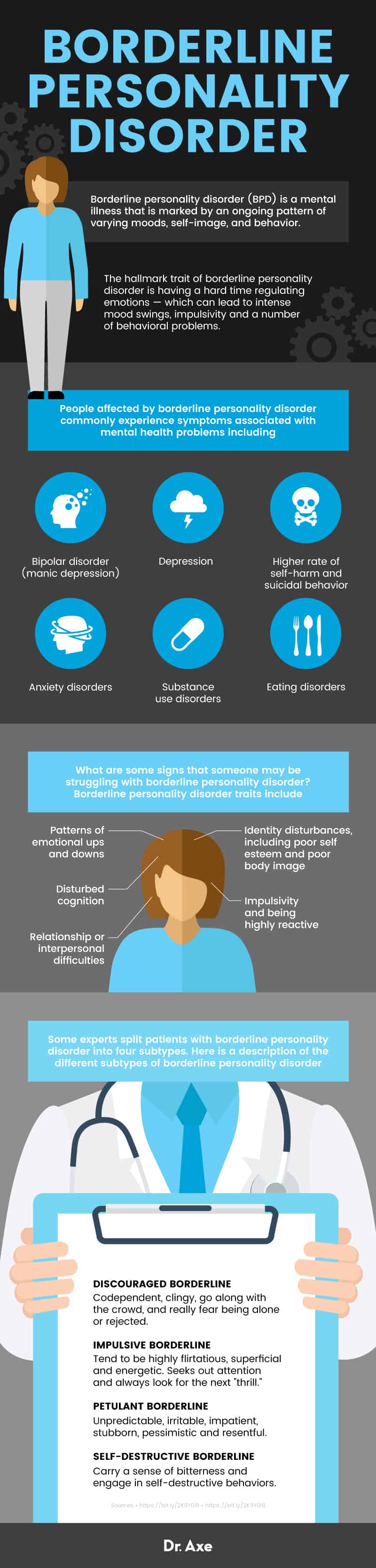
Maybe someone you know is struggling with borderline personality disorder. The hallmark trait of borderline personality disorder is having a hard time regulating emotions — which can lead to intense mood swings, impulsivity and a number of behavioral problems. Borderline personality disorder (BPD) is one of the most common mental disorders that adults experience. According to the National Alliance on Mental Health, “It’s estimated that 1.6 percent of the adult U.S. population has BPD, but that number may be as high as 5.9 percent. Nearly 75 percent of people diagnosed with BPD are women.” (1)
How serious is borderline personality disorder? It’s very different than someone experiencing some ups and downs in their moods, which is common and can even be considered normal. Borderline personality disorder can be very serious at times, even leading to depression and suicidal thoughts or behaviors, especially in adolescents. (2) People with BPD are also more likely to harm themselves via substance abuse, acts like cutting, and potentially life-threatening eating disorders like anorexia nervosa or bulimia nervosa. In psychiatric settings, as many as 15 percent to 20 percent of all patients are believed to have BPD.
First-line treatment for borderline personality disorder involves therapy, support from family and friends, and, sometimes, medication. There are also many natural ways to help manage BPD symptoms, which include: eating a healthy diet, exercise, many different stress-releiving activities, and supplements that help reduce deficiencies.
What Is Borderline Personality Disorder?
The definition of borderline personality disorder is “a mental illness that is marked by an ongoing pattern of varying moods, self-image, and behavior.” (3)
Personality traits that are common among people with BPD include: anxiety, insecurity and poor self-image, unhealthy relationships, anger, self-harm, and instability. After an event that is upsetting or “triggering,” people with BPD have a difficult time coping and calming down (what some refer to as a “hard time returning to a stable baseline”). Experts consider borderline personality disorder to be a “major public health problem” because it’s associated with high levels of mental health service use and serious psychosocial impairment. (4)
What are some signs that someone may be struggling with borderline personality disorder? Borderline personality disorder traits include:
- Patterns of emotional ups and downs
- Impulsivity and being highly reactive
- Relationship/interpersonal difficulties
- Identity disturbances, including poor self esteem and poor body image
- Disturbed cognition
Signs and Symptoms
The Diagnostic and Statistical Manual, (5th Edition), aka the “DSM-5” that is used by psychologists/psychiatrists, includes a certain criteria/framework that is used to diagnose borderline personality disorder. Diagnosis is based on specific personality traits, signs and symptoms. The DSM-5 states that “The essential features of a personality disorder are impairments in personality (self and interpersonal) functioning and the presence of pathological personality traits.”
In the past (as of the year 2000) there were nine symptoms that were used to officially diagnose BPD. To make a diagnosis, someone’s symptoms had to include at least five of the following nine symptoms: (5)
1. Making effort to avoid real or imagined abandonment by friends and family.
2. Unstable personal relationships. It’s typical for relationship status to fluctuate between feelings of love and hate.
3. Distorted and unstable self-image. Poor self-esteem affects moods, values, opinions, goals and relationships.
4. Impulsive behaviors. These can include excessive spending, unsafe sex, substance abuse or reckless driving.
5. Self-harming behavior, such as cutting or suicidal threats and attempts.
6. Periods of intense depressed mood, irritability or anxiety. These can last between a few hours to a few days.
7. Chronic feelings of boredom or emptiness.
8. Inappropriate, intense or uncontrollable anger. After an angry episode it’s common for shame and guilt to be felt.
9. Cognitive disturbances. This can include dissociative feelings, or disconnecting from your thoughts or sense of identity. Sometimes stress-related paranoid thoughts/psychotic episodes can also occur.
The official borderline personality disorder criteria has changed a bit since 2013. The criteria for BPD now includes:
1. Significant impairments in personality functioning:
- Self identity impairment — Poorly developed, or unstable self-image, often associated with excessive self-criticism, chronic feelings of emptiness, and dissociative states under stress)
- Lack of self-direction — Instability in goals, aspirations, values or career plans.
- Impairment in interpersonal functioning — having reduced ability to recognize the feelings and needs of others associated with interpersonal hypersensitivity (i.e., prone to feel slighted or insulted).
- Problems with intimacy — Intense, unstable, and conflicted close relationships, marked by mistrust, neediness and anxious preoccupation.
2. Pathological personality traits in the following domains:
- Emotional Instability — Unstable emotional experiences and frequent mood changes. Emotions that are easily aroused, intense, and/or out of proportion to events and circumstances.
- Anxiousness — Intense feelings of nervousness, tension or panic, often in reaction to interpersonal stresses. Feeling fearful, apprehensive or threatened by uncertainty or losing control.
- Separation insecurity — Fears of rejection, excessive dependency and complete loss of autonomy.
- Depressivity — Frequent feelings of being down, miserable, hopeless, difficulty recovering from such moods, pessimism about the future, potential suicidal thoughts.
- Impulsivity — Acting on the spur of the moment responses.
- Risk-taking — Engagement in dangerous, risky and potentially self-damaging activities.
- Antagonism and hostility — persistent or frequent angry feelings, even in response to minor insults.
Some experts split patients with borderline personality disorder into four subtypes. Here is a description of the different subtypes of borderline personality disorder: (6)
- Discouraged Borderline — Codependent, clingy, go along with the crowd, and really fear being alone or rejected.
- Impulsive Borderline — Tend to be highly flirtatious, superficial and energetic. Seeks out attention and always look for the next “thrill.”
- Petulant Borderline — Unpredictable, irritable, impatient, stubborn, pessimistic and resentful.
- Self-Destructive Borderline — Carry a sense of bitterness and engage in self-destructive behaviors.
Causes and Risk Factors
What are the main causes of borderline personality disorder? Like other mental illnesses, BPD is believed to be caused by a combination of genetic, lifestyle and environmental factors — rather than one single cause.
Women are much more likely to be diagnosed with BPD than men. However, some experts believe that just as many men as women are actually affected by BPD, but men may be more likely to be misdiagnosed with post traumatic stress disorder (PTSD) or depression.
Experts believe that factors that contribute to borderline personality disorder can include:
- Inheritance, family history and genetics — Research suggests that BPD has strong hereditary links and is about five times more common among people who have a first-degree relative with the disorder. Studies show that there’s an estimated heritability of approximately 40 percent among people with BPD. (7)
- Early traumatic life events — Examples of trauma that contribute to mental illnesses include physical or sexual abuse during childhood, neglect, death in the family, and separation from parents.
- Impairments in brain function — Studies have found evidence of a neurological basis for some BPD symptoms. For example, some investigational studies have found in people with BPD the “emotional regulation system” of the brain doesn’t seem to work properly, which affects decision-making, judgment, communication, cooperation and behaviors towards others. There’s also evidence of differences in the volume and activity in brain structures related to emotion regulation between people with BPD and those without it. (8) Is a chemical/neurotransmitter imbalance to blame for BPD? Certain meta-analyses have found that in people with BPD there’s “no significant associations found for the serotonin transporter gene, the tryptophan hydroxylase 1 gene, or the serotonin 1B receptor gene.”
Can you develop borderline personality disorder at any age? Yes, although BPD is usually diagnosed in young adulthood, such as in someone’s teens, 20s or 30s. In most cases, symptoms begin by early adulthood and then remain present in a variety of contexts/situations.
Co-morbidities of Borderline Personality Disorder:
If you have BPD, you’re more likely to struggle with other behavioral/mental problems too. This can make BPD difficult to treat, since it can lead to life feeling like it’s spiraling out of control. People affected by borderline personality disorder commonly experience symptoms associated with mental health problems including:
- Depression
- Bipolar disorder (manic depression)
- Higher rate of self-harm and suicidal behavior
- Anxiety disorders
- Substance use disorders
- Eating disorders
Conventional Treatment
There is no official borderline personality disorder test that doctors use to make a diagnosis. BPD is diagnosed by mental health professionals after they carry out a clinical interview with a patient, review their symptoms and medical history, discuss family history of mental illnesses, and sometimes interview family or friends to discuss any relationship and behavioral struggles.
Can you cure BPD? Borderline personality disorder is a condition that can definitely be managed, but will usually stick with someone throughout their lifetime. Symptoms will usually improve with treatment, but can get worse again during very stressful times or if treatment is stopped. To be effective, BPD treatment must also address other existing mental health conditions that a patient’s facing, such as depression and substance abuse.
Treatment options for borderline personality disorder can include any combination of the following:
- Psychotherapy (or talk therapy), especially Dialectical Behavior Therapy (DBT), which was specifically developed for individuals with borderline personality disorder. (9) DBT uses concepts of mindfulness meditation and acceptance to work through destructive reaction patterns. Another type of therapy that is used to manage BPD is Cognitive Behavioral Therapy (CBT). CBT has the goal of identifying and changing core thoughts/beliefs that lead to problematic behaviors and inaccurate perceptions.
- Family therapy or group support may be used. For example, group therapy is a common treatment in the case of substance abuse or eating disorders.
- In some cases, use of medications. Because studies haven’t shown that neurotransmitter imbalance is a core underlying cause of BPD, medications are not typically used as the primary treatment. However, if a patient is struggling with depression, anxiety or psychotic episodes, their doctor might prescribe medications to help treat specific symptoms. This can include antidepressants such as SSRIs, or selective serotonin-reuptake inhibitors. Medications can be useful for temporarily reducing symptoms like mood swings, insomnia and depression, but they are very unlikely to “cure” borderline personality disorder.
- If needed, outpatient treatments, hospitalization or emergency care may be used to stabilize a patient who is experiencing severe distress or suicidal thoughts.
Ways to Help Borderline Personality Disorder Treatment
1. Therapy or Counseling
Therapy, including DBT, CBT or family therapy, is considered “first-line treatment” for people with borderline personality disorder because it can help to manage destructive thought patterns and behaviors. Psychotherapy takes place between a patient and a licensed and trained mental health care professional who can help point out underlying problems and offer solutions. Sometimes family members (spouses, parents or kids) or close friends may also attend therapy sessions for support.
There are many different types of therapy, and it’s common for therapists to combine and adapt elements of different approaches. DBT is popular for treating BPD because it’s been one of the most studied types of therapy. In certain clinical studies, DBT has been shown to help reduce suicidal behavior and self-injury, inpatient hospitalization, and treatment drop out better than other treatment options. (10) The most effective DBT approaches include about one hour of weekly individual therapy, a two-hour group skills training session, out-of-session communication as needed, and a consultation between the patient’s other doctors and their therapist. Studies have also shown shorter workshops and training sessions (about 90 minutes to three hours long) on different therapy approaches to be helpful for patients with BPD.
Some of the goals of therapy for treating BPD include learning how to better:
- Realistically think through perceptions about oneself and others. Therapy helps the patient become aware of ways of thinking that may be automatic but inaccurate and harmful. DBT and CBT are useful for questioning thoughts and understanding how they affect emotions and behaviors.
- Interact with others in a way that helps maintain healthy relationships.
- Develop skills to better understand how to deal with stress.
- Effectively express feelings and emotions.
- Control intense reactions to stressful situations.
- Reduce self-destructive behaviors, especially substance abuse and suicidal thoughts.
- Reduce impulsivity and aggression.
- Better-recognize warning signs and plan how to prevent an episode using coping strategies.
- Manage mood swings, depression, hopelessness, anger and anxiety. Relaxation exercises, guided meditations, mind-body practices and mindfulness techniques may be used to gain control over stress-induced reactions.
- Build skills in goal setting, healthy eating, sleep, exercise habits, and general self-harm avoidance.
If family and/or friends attend therapy sessions, this is helpful for offering emotional support and gaining more understanding, patience and encouragement. Improving relationship skills is important for reducing fighting and anxiety over being rejected or neglected, which is a common trait among people with BPD.
Other types of therapies might be most effective if co-morbidities need to be treated, such as PTSD, substance abuse or eating disorders. For example, DBT plus prolonged exposure protocol (DBT-PE) has been shown to help people with PTSD and BPD, while three-month inpatient treatment using DBT has been shown to help those with eating disorders plus BPD. Other types of therapy that are sometimes recommended for borderline personality disorder treatment include Mentalization-Based Treatment (MBT), Transference-Focused Psychotherapy (TFP) and Schema-Focused Therapy (SFT). (11)
2. Help Treat Depression
Some of the most common and concerning borderline personality disorder symptoms are those associated with depression, such as hopelessness, isolation and self-harm. If depression is something you deal with, consider if any of these underlying depression causes might apply to you:
- Chronic stress from things such as financial or job related problems
- Unresolved emotional problems from childhood
- Neurotransmitter imbalance
- Hormonal imbalances
- Unresolved food allergies
- Alcoholism or drug use
- Nutrition deficiencies
- Lack of sunlight
- Toxicity from metals or mold
Identifying factors that contribute to your depression can help you or your therapist to come up with an effective treatment plan. Ways that you can help naturally treat depression symptoms include:
- Eating an anti-inflammatory diet (more on this below). Avoid processed foods that can contribute to fatigue or mood swings, including foods with added sugar, sweetened drinks and desserts, fried food, processed meats, refined grains and low-quality dairy products.
- Getting daily exercise, especially outdoors. Exercise is a natural mood-lifter and also has anti-inflammatory and pain-reducing effects. Try exercises such as walking, cycling or another type you enjoy for 30–90 minutes daily.
- Avoiding alcohol, drug use or even too much caffeine.
- Treating nutrient deficiencies, such as vitamin D deficiency, magnesium deficiency or low intake of omega-3 fatty acids. I recommend taking a quality multivitamin, vitamin D3, probiotic supplement, and omega-3 fatty acid supplement daily.
- Consider taking St. John’s Wort, a natural herb that works in a similar way as selective serotonin reuptake inhibitors (SSRIs) for lifting your mood.
- Seek support from family, friends and your community. Find a strong group of friends that you can share your struggles with; joint a support group online or in person; or consider joining a spiritual group or community.
- Spend more time in nature. Aim to spend at least 10–20 minutes in the sun daily to lift your mood and prevent vitamin D deficiency.

3. Manage Anxiety
Anxiety can exacerbate borderline personality disorder by leading to social isolation, difficulties completing tasks, poor self image, use of drugs or alcohol, and so on. Try these remedies for anxiety to help you feel calmer and more in control:
- Seek out a therapist who specializes in art therapy, music therapy or mindfulness practices.
- Try biofeedback therapy, which helps you relax your body in response to stress/anxiety.
- Exercise daily.
- Avoid stimulants, including alcohol, drugs and even certain medications.
- Take adaptogen herbs, which are a class of healing plants that improve your ability to deal with stress, balance hormones such as cortisol, and help with relaxation. Adaptogens that may help treat anxiety and depression include rhodiola, kava root and ashwagandha, which work by increasing the sensitivity of your neurons, including two important neurotransmitters that regulate your moods: serotonin and dopamine.
- Use lavender and chamomile essential oils, which are natural remedies for improving calm feelings and relaxation. You can add 5–10 drops to a warm bath, diffuse 5–10 drops in your bedroom at night to promote sleep, or apply 2–3 drops topically to your skin (such as your temples, chest and wrists).
- Create a “bed time” routine to help you unwind at night. If you struggle to get good sleep, natural sleep aids that can help include: making your bedroom very dark and slightly cool, reading something calming, journaling, taking a warm shower or bath with Epsom salts, self massage, meditation, prayer, breathing exercises, taking a magnesium supplement, or drinking calming tea.
- Keeping a calendar or daily planner to avoid missing meetings or feeling overwhelmed.
- Taking breaks throughout the day to rest, nap or meditate.
- Take a magnesium supplement and B-vitamin complex. You can also speak with your therapist or doctor about taking GABA or 5-HTP supplements, which are derived from natural amino acids that support mental health. They have natural calming effects but should not be taken with any prescription anti-anxiety or antidepressant medications.
4. Lifestyle Changes
Get enough sleep and rest (aim for seven to nine hours of sleep per night) to help prevent fatigue and mood swings. It can be helpful to stay consistent with a regular sleep-wake routine so that your circadian rhythm (or “internal clock”) gets more normalized. It’s also important to eat a nutrient-dense diet that helps fight depression and anxiety. Whole foods that should be part of your diet to prevent and treat mood-related problems include:
- Omega-3 foods, which help to reduce inflammation and support brain function. The best omega-3 foods include wild-caught fish like salmon, mackerel, herring and white fish, walnuts, chia seeds, flaxseeds, natto and egg yolks.
- Fruits and vegetables, which increase your intake of antioxidants and vital nutrients that support your mood and prevent deficiencies. Some of the best to include in our diet are: leafy greens like kale or spinach, asparagus, avocado, beets, broccoli, carrots, peppers, tomatoes, mushrooms, blueberries, goji berries, blackberries, cranberries and artichokes.
- Healthy fats, which provide important vitamins and minerals that boost energy levels and mood. The best options are: avocados, grass-fed butter, coconut oil, extra virgin olive oil and omega-3s like walnuts and flaxseeds. Avoid consuming trans fats (like hydrogenated oils) and processed vegetables oil, which can promote inflammation.
- Clean protein sources, which are critical for supporting neurological function and balancing hormones. The best sources of protein include grass-fed beef, lentils, wild fish, organic chicken, black beans, yogurt, free-range eggs, raw cheese and protein powder made from bone broth.
- Probiotic foods that support gut health, cognitive function and production of neurotransmitters. Some of the top probiotic foods include kefir, yogurt, kombucha, miso, raw cheese and fermented vegetables. In fact, a great way to consume probiotics is to drink kombucha every day because it also contains enzymes and B vitamins that boost your energy levels and help to detoxify your body.
Precautions
If you know someone with borderline personality disorder who is having suicidal thoughts or thinking of harming themselves, reach out for help right away. You or the affected person can call the toll-free National Suicide Prevention Lifeline (NSPL) at 1-800-273-TALK (8255), 24 hours a day, seven days a week for counseling and help for free.
If you yourself are experiencing any of the following symptoms, consider speaking with a therapist who can help guide you toward treatment and recovery:
- Overwhelming sadness or helplessness
- Insomnia
- Difficulty focusing on work or at school
- Trouble carrying out everyday activities
- Constant worry
- Using drugs or drinking to excess
- Feeling very overwhelmed during a difficult life transition, such as a divorce or job change
For help finding a mental health provider in your area, you can refer to the Help for Mental Illnesses page on the National Institute of Mental Health’s website.
Final Thoughts
- Borderline personality disorder (BPD) is a mental illness that is marked by an ongoing pattern of varying moods, self-image, and behavior.
- Signs/traits of borderline personality disorder include: avoiding abandonment, unstable personal relationships, distorted and unstable self-image, impulsive behaviors, self-harming behavior, periods of intense depressed mood, chronic feelings of boredom or emptiness, inappropriate anger, and cognitive disturbances.
- Underlying causes that can contribute to BPD include: genetics/inheritance, early traumatic experiences, substance abuse, and abnormal brain function.
- Co-morbidities can make BPD difficult to treat. These include: depression, anxiety, PTSD, eating disorders and substance abuse.
Read Next: Dysthymia: Coping with Chronic Depression + 7 Mood Boosters








